Tell us something about yourself, and your background:
- I am a surgeon and critical care specialist. During the first half of my thirty-plus years of practice, I was Chief of Trauma Surgery and Critical Care at a major New York academic medical center. I started and supervised a productive trauma research lab, authoring dozens of NIH-funded papers. As I grew older, my surgical practice grew to involve all aspects of minimally invasive surgery, including advanced cancer procedures. My passion outside the operating room, however, has always been the education of future surgeons. I designed and taught 2 of the first advanced surgical anatomy courses. My students have gone on to be Chairmen of surgical departments at major academic medical centers, as well as skilled practitioners and clinicians. However, I found that our methods of surgical training were progressively failing to educate our students and residents in the advancing technology of surgery. Five years ago, I was forced to give up surgical practice due to a sudden visual disability. At that moment, I devoted myself to full-time to advancing the education of surgery.
List your ventures with a brief explanation of each:
- Before starting ParaSurgical Systems, I was Chief of Trauma Surgery. My passion has always been surgical education and training. As part of this work, I designed curriculum and taught surgical anatomy. I’ve done both laboratory research and clinical research. I’ve designed and patented multiple surgical devices. I’ve authored a textbook on Shock and Resuscitation and am currently completing a textbook on Minimally Invasive Surgery. I’ve presented papers and Grand Rounds lectures nationally and internationally. But now, my complete focus is on my new company and the design of a revolution in surgical training.
How did you get to where you are? What set you off?
- For over thirty years, I’ve trained the next generation of surgeons. While the practice of surgery has advanced dramatically during this time, we continue to teach surgeons in the same operating room mentorship style that has existed for over a century. As a result, surgical training is currently in crisis. Less than half of our graduates are certified as competent in robotically assisted surgery. In the US, over 30% of surgical procedures result in complications. This trend will only worsen in the coming decades, with a profound and increasing shortage of adequately trained surgeons projected for 2035. I realized that teaching residents how to become great surgeons one at a time was no longer good enough. I knew that there was a better way to train–the same realization that led the airline industry to adopt advanced simulation to train commercial pilots. I started a company to pursue the development of an equivalent, high-fidelity simulation for surgeons.
Tell us a bit more about each of your ventures:
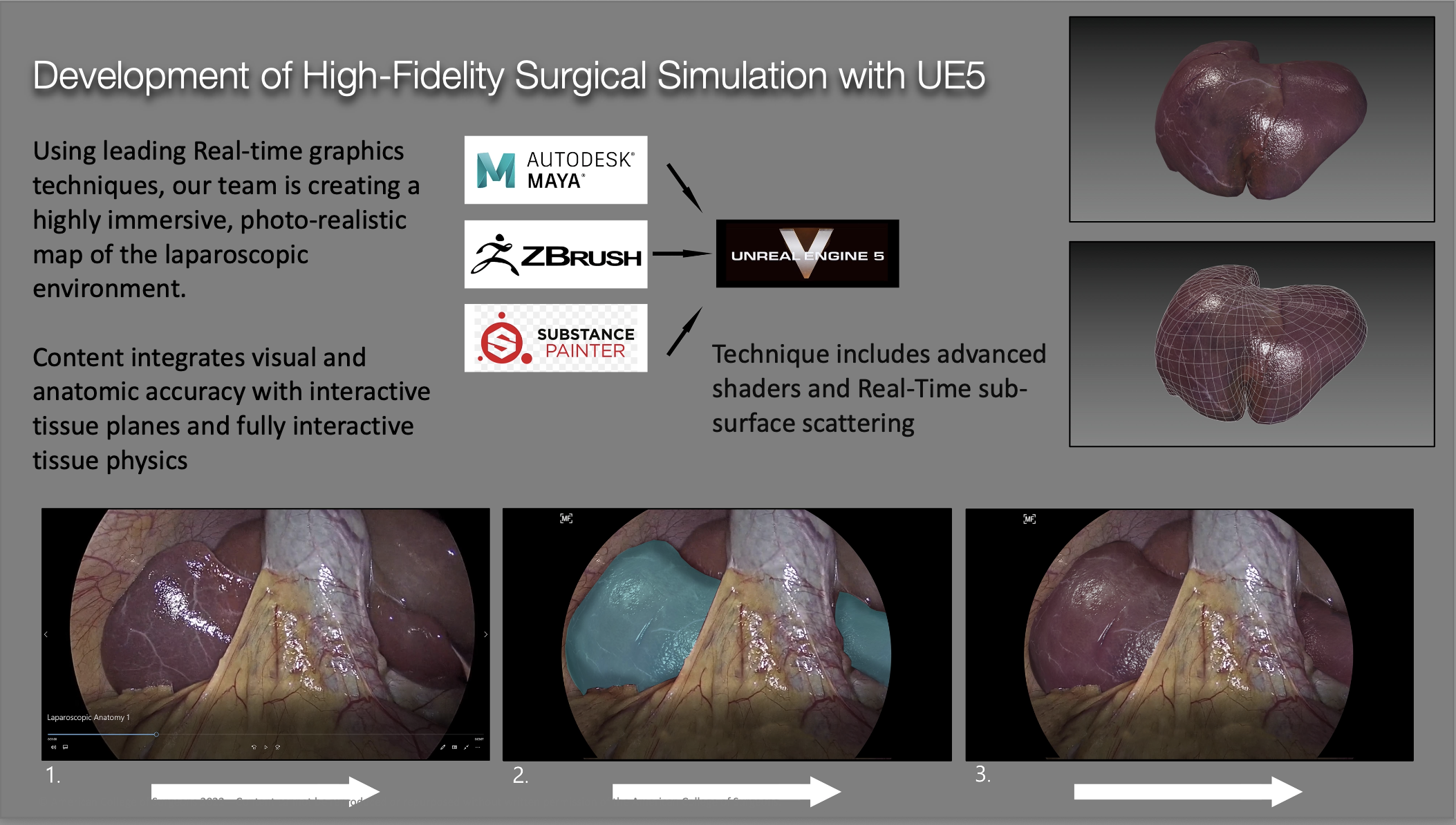
- I realized that nobody was trying to do what I was doing. I knew that the creation of a simulator was possible, however, because I was familiar with the recent advances in game technology. I was convinced that the latest graphics engines were nearly capable of what I needed, though they had never been employed to train surgeons. I pitched the idea of using AAA gaming technology to develop something a little more socially redeeming than another first person battle royale, and was able to secure my first funding from a game engine developer. I leveraged my limited funds by partnering with DigiPen Institute of Technology, and was able to work with brilliant artists and game engineers, many still pursuing their education. Over the next three years, we built the precesses and pipelines to create the basis for a truly immersive surgical simulator. Two years ago, my co-founder, Stan DeMarta, joined the company. Stan has a strong med tech and engineering background and is an experienced and successful entrepreneur. With his help, we have advanced ParaSurgical Systems to where it is today.
Any other information:
- This journey has brought us to the point where we know we can achieve our goal of revolutionizing surgical training. Patients shouldn’t be exposed to the early training of surgeons, and with our new technology, this will no longer be the case. Surgeons will finally be able to train for all manner of emergencies and unusual anatomic variations. We will finally have a system to objectively evaluate the skills of surgeons as they advance in their careers. We’ll even be able to incorporate a patient’s MRI and CT scan data into our simulation, so that surgeons can practice difficult procedures before putting the patient at risk. The first few steps have been taken. Now, the challenge is to find the funding to complete the journey.


